Glaucoma Laser Therapy
Energy to Glaucoma care
Pioneer of SLT Technology
Open-angle glaucoma threatens the sight of more than 50 million people worldwide, with the number of annual cases significantly on the rise. This means glaucoma patients are an increasingly important part of any practice. Lumenis offers an array of ophthalmic laser systems that continue to provide the ophthalmologist with essential surgical tools to help lower intraocular pressure and control this progressive, degenerative disease.
A minimally invasive technological breakthrough, the Smart Selecta Duet glaucoma laser system is changing the future vision of glaucoma patients with Selective Laser Trabeculoplasty (SLT). SLT provides the benefits of Argon Laser Trabeculoplasty (ALT) without the coagulative damage that leads to scarring. From photocoagulators to photodisruptors, Lumenis’ family of advanced laser technologies are an invaluable mainstay in the treatment of glaucoma.
How & Why It Works?
ALT spot size (left arrow) vs. SLT spot size (right arrow) on TM
Since Selective Laser Trabeculoplasty depends on the laser parameters for targeting the pigmented cells, it is not necessary to have a small spot size or to precisely target a site in the trabecular meshwork as compared to traditional Argon Laser Trabeculoplasty.
For SLT a large 400 micron spot is directed into the angle using a specially developed gonio lens to minimize beam distortion and provide good visualization of the angle. Unlike ALT, focus is not critical since the large spot has a greater depth of focus than the 50 micron ALT spot. A red aiming beam the same size as the treatment beam shows the area to be treated. Selective Photothermalysis determines which cells are targeted and activated.
During treatment there is normally no observable tissue reaction. Due to variations in pigmentation the laser energy is normally adjusted to a level just below that where a minimally observable effect is achieved.
The underlying mechanism is selective photothermalysis that enables the laser to precisely target intracellular melanin granules to activate individual cells while not disturbing adjacent non-pigmented cells. The activated cells release cytokines that trigger a targeted macrophage response to the trabecular meshwork cells. The macrophages reactivate the meshwork reducing fluid outflow resistance and lowering intraocular pressure.
For SLT the light energy is provided by a specially designed Q-switched, frequency doubled Nd:YAG laser operating at 532nm green with an output of from 0.3 to 1.5 millijoules.
The target tissue is melanin granules within individual trabecular meshwork cells. Based on the size of the pigment granules, it is necessary to deliver the light energy within 1 microsecond. The Q switched laser pulse width is 3 nanoseconds, well within the required time interval to contain the energy and temperature rise to the pigment granules. Mark Latina, M.D. inventor of SLT did cell culture and animal experiments to determine the specific energy range for selective cell damage. (Click here for Latina paper) Through his investigation parameters were determined which would activate certain pigment containing meshwork cells while sparing immediately adjacent non-pigmented cells. Further human studies showed the pressure lowering effects of Selective Laser Trabeculoplasty without observable damage to the trabecular meshwork cells.
Fluorescent live/dead assay reveals that only melanin-laden trabecular meshwork cells are affected, as seen with red nuclear staining.
Selective Laser Trabeculoplasty is an improvement over conventional ALT by eliminating thermal damage of the trabecular meshwork architecture.
Using a low-energy, Q-switched, frequency doubled Nd:YAG laser emitting at 532 nm with a pulse duration of 3 nanoseconds, researchers demonstrated isolated destruction of the pigmented TM cells without thermal or collateral damage to the surrounding non-pigmented cells and trabecular collagen beams. Further, endothelial membrane formation on the TM, usually found in ALT-treated eyes, was not observed after SLT exposure in vivo.
Other research using scanning and transmission electron microscopy to compare the acute morphologic changes in the TM of human eye bank eyes after ALT and SLT confirmed these histologic findings. After laser irradiation, ALT produced crater formation, coagulative damage, fibrin deposition and disruption of trabecular beams and endothelial cells. Eyes treated with SLT did not show these findings; the general structure of the TM was preserved. SLT’s effect occurred intracellarly, with disruption of the melanin granules. The lack of thermal and structural damage to the TM makes SLT potentially repeatable.*
* Source: Review of Ophthalmology, April 2001, David A. Lee, MD & Peter A. Netland, MD, PhD, pgs. 1-2
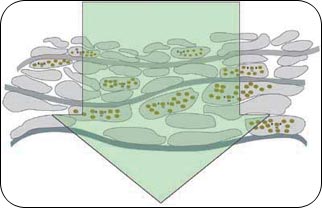
Representation of 400 micron SLT laser beam penetrating through TM
The in vitro and in vivo findings after SLT are due to the much shorter pulse duration (3 nanoseconds) of the treatment compared to the thermal relaxation time of the target chromophore (melanin) in the pigmented TM cells. The melanin granules have a thermal relaxation time of approximately 2 microsecond, while the pulse duration of the SLT is 3 nanoseconds. This means that the pulse duration of SLT is too short for the melanin to transfer the thermal energy; and consequently this spares the surrounding tissues from damage. *
* Source: Review of Ophthalmology, April 2001, David A. Lee, MD & Peter A. Netland, MD, PhD, pgs. 1-2
Lumenis SLT – Procedure Video
FAQ
Physicians and patients are benefiting from the SLT procedure in the following ways:
Pre-Op
Preoperatively, careful goinoscopy should be done to visualize the trabecular meshwork and plan the treatment area.Preoperative medications consists of a drop each of lopidine or Alphagan and topical anesthesia. A SLT laser gonio or zero magnification lens is placed on the eye with methylcellulose. The aiming beam is focused onto the pigmented trabecular meshwork.
During
Treatment is done in single-burst mode, placing 50 ± 5 contiguous, but not overlapping, 400-micrometer laser spots along 180 degrees. Bubble formation is monitored with each pulse. In cases with significant variation in trabecular pigmentation, the pulse energy is decreased if bubble formation occurred as described above.
Post-Op
After laser treatment, prednisolone acetate 1% is administered and continued n the treated eye four times daily for four to seven days.
* Source: SLT Evolves as a Treatment For Open-angle Glaucoma, Review of Ophthalmology, David A. Lee, MD & Peter A. Netland, MD, PhD, April, 2001, p. 3)
PB-2006798 Rev A